It’s no secret, drug overdoses in America are increasing. In terms of drug overdose deaths, 2020 was one of the worst years on record. In this past year over 93,000 people died, an increase of nearly a third over 2019 and a dark shadow around an already dark year as we deal with the ongoing pandemic. While the stresses of the pandemic drove a significant amount of the increase in drug use, as much of the deaths, if not more, have been driven by contaminations in the supply of drugs throughout the nation.
One of the key things that increases both demand for mental health services and substance use disorders is any increase in uncertainty and stress in the world around a person. With many folks’ jobs shut down, state assistance programs delayed, unclear, or unavailable, health concerns, and civil unrest it should be no surprise that 2020 was stressful and rife with uncertainty. The CDC stated that in June 2020 as many as 13% of Americans had said that they started using substances or increasing substance use to cope with the stresses of the pandemic. Nearly every state in the nation saw an increase in substance use disorders this year.
Many people, due to the shifts in habits, safety, and other issues, found that the substances that they were usually using were harder to access according to Dr. Mandy Owens at the Alcohol and Drug Abuse Institute. Many people in crisis have been looking for any way to escape the stress of their circumstances, and in this are willing to turn to more extreme measures or to new dealers in these times of crisis.
However, those numbers don’t seem on the face of them to add up to a 30% rise in deaths, so what else is going on?
The Specter of Fentanyl

Most people dealing drugs illegally are opportunistic in nature, and don’t have a devoted space to portion out different drugs cleanly. Often, hashing out drugs of different types are done on the same tables, with poor labelling, and this leads to cross contamination. Someone who has any amount of fentanyl that they are dealing is likely to spill onto the common space and get mixed in with other products. Because drugs are expensive, when dealers clean up their spaces, they are trying to recover every bit of product that they can and so these mixed spills are collected, packed up, and sold as if they were just one product when in fact they are not.
These economic realities of drug dealing mean that people who are already abusing substances often cannot know with 100% certainty what they are getting. This is more than a little important as mixing different drugs with different health conditions or other substances can be lethal by itself. Add to that the fact that a lot of people with substance use disorders have been affected by the economic troubles of the pandemic, and thus are less likely to be able to choose between a more careful dealer and a less careful one, along with the increased time and decreased opportunity of being unemployed during the pandemic, you have a perfect storm for unexpected fentanyl overdoses.
And that is exactly what we’ve seen. In 1970, during the heroin epidemic throughout U.S. cities, we saw 7,200 overdose deaths, 13 times less than we saw this year. Our current epidemic of opioid overdoses is unique in the history of the nation, and it has been accelerated by the situation that we currently find ourselves in. To get out of it is going to require a foundationally different approach than we have used in the past.
Decreasing Access to Help
At the same time that the pandemic was driving people to use more, it also cut people off from a lot of the systems that they were using to address their substance use disorders. At the most basic level, people trying to avoid others who lived alone were less likely to have someone around when an overdose happened. People passing by have been less likely to risk contact to administer emergency care. And many people were avoiding the hospital altogether for fear of catching COVID-19.
As we move out from emergency care, we also see another circle of support that was denied to people this year. During the pandemic, many people’s in-person support groups shuttered or moved online in a way that was less accessible, despite best efforts of professionals working with these communities. Many people discontinued their methadone treatments due to COVID-19 and some physicians were less likely to send people to methadone clinics due to the difficulties of COVID-19. This means that people were less able and less likely to get assistance with severe, recognized substance abuse in the ways that they were before the pandemic.
One upshot of all of this difficulty though is that more people have figured out how to deliver assistance at a distance in terms of group therapy. Narcotics Anonymous and Alcoholics Anonymous both have figured out how to transition to an online presence, and many other systems have worked out the kinks in implementation as well. Hopefully this will create significantly increased access to group therapy for people in the future and some good can come out of this year’s disruption of care.
What Is An Overdose Exactly?
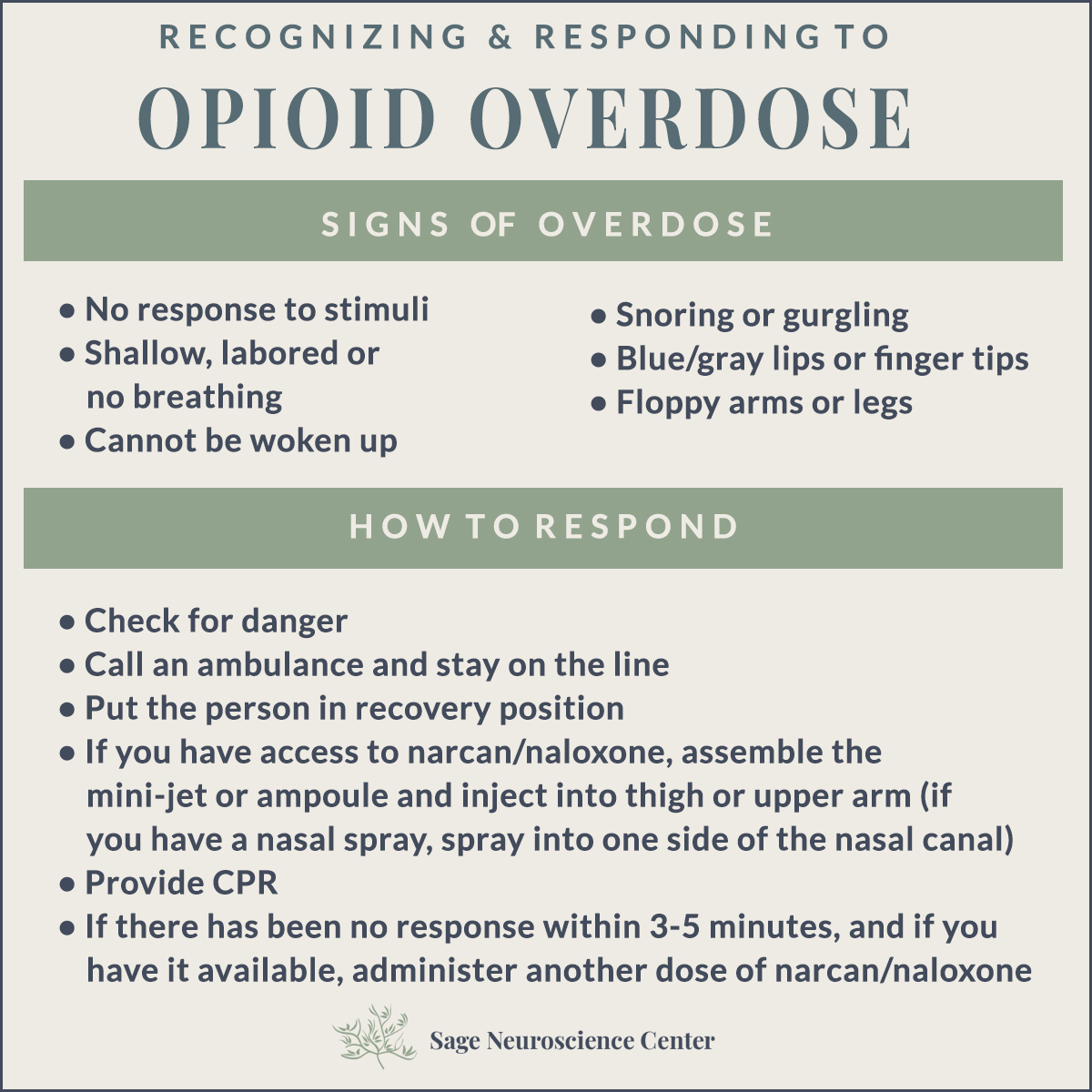
Overdose symptoms can be quite diverse but they primarily center around disruptions of the central nervous system (CNS) and people who die by overdose most commonly die due to respiratory failure either due to choking or due to their CNS being overwhelmed and their brain forgetting to send signals to their limbs. Overdoses come in two main different types, however, and it is important to be able to distinguish between them:
- Depressants such as alcohol, opioids, and benzodiazepines all lower blood pressure and body temperature by adjusting the central nervous system. In overdose, they cause sedation and eventually respiratory failure. This is recognizable as someone being unresponsive to attempts to rouse them and warrants immediate attention.
- Stimulants such as meth or cocaine accelerate the central nervous system, increasing blood pressure, body temperature, heart rate, and breathing. In overdose conditions, stimulants provoke a wide array of symptoms causing the cardiovascular, respiratory, and circulatory systems to overwork themselves and collapse. This can be recognized as jerking limbs, high fever or pulse, seizures, chest pain, headaches, unconsciousness, and heart attack.
Recognizing what is going on and acting quickly can be the difference between life and death for someone in overdose.
Is It Time for Opioid Detox? Take the Quiz
What’s Involved in Overdose Treatment?
For stimulant overdoses, there is little to nothing a person without significant training can do for someone, aside from keep calm and contact emergency services. No matter what a person says, an overdose is a matter of life and death, and getting them into the care of doctors with appropriate medication can save their life. At any hospital in America, medications exist to stabilize people’s blood pressure, treat heart attack, reduce body temperature, and machines exist to support respiratory issues. However, these are not treatments that non-medical professionals are able to give someone, so the single-most important step is to contact emergency medical services immediately.
On the other hand, in the case of real or suspected opioid overdose there is one thing that you should absolutely do first: naloxone should be administered as quickly as possible even if you are not 100% sure that it’s an opioid overdose. Naloxone has no known negative interactions, and when it comes to opioid overdoses, seconds matter. No-one should be mad at you for administering naloxone if you have it. This is the first thing that any medical professional will do upon arriving, and it is also the first thing you should do if anyone in the area has it. For many opioid overdoses, naloxone alone can be sufficient to save someone’s life.
Where to Get Naloxone?
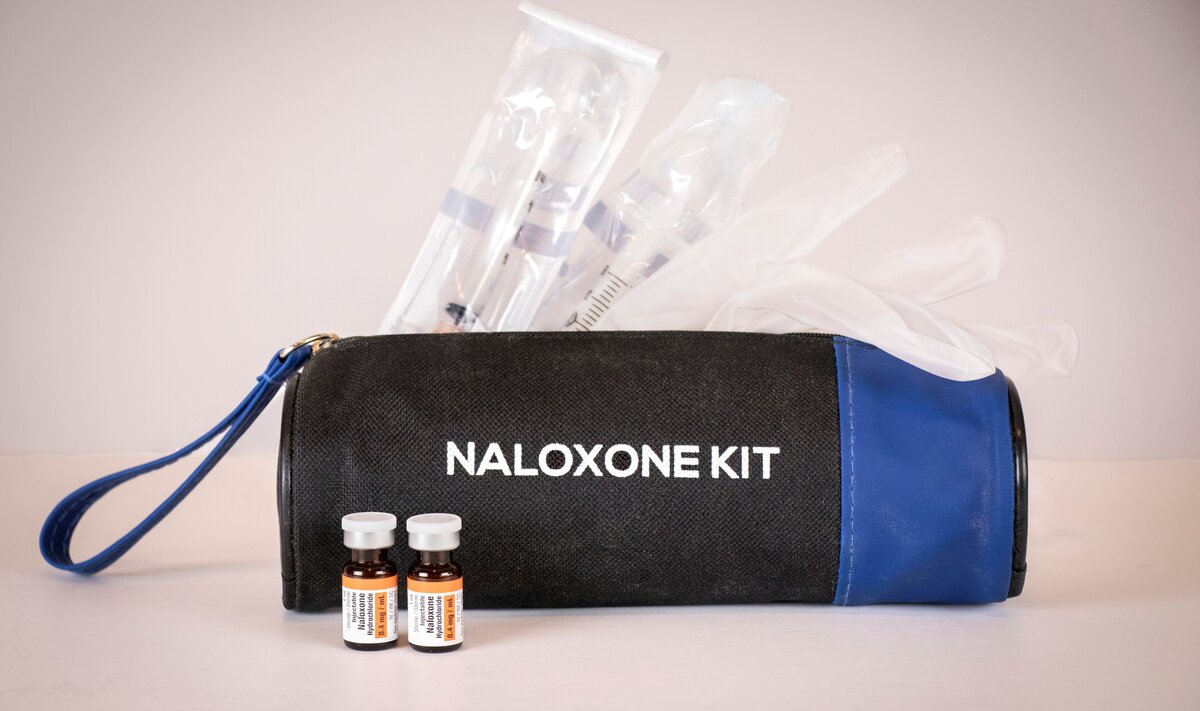
Even in states that don’t have free naloxone, if you know someone who is believed to be at risk of an opioid overdose, doctors can offer a third-party prescription so that you can have it on hand in case anything happens.
How Does Naloxone Work?
Naloxone works by binding to the same opioid receptors in your brain that the chemical causing the overdose is bound to. Naloxone grabs onto these receptors and knocks off the opioid in question, preventing it from triggering the responses that make it dangerous to the body. This effect is temporary and harmless, though disconcerting at first.
Moving Out of the Darkness
Due to the combined problems of the opioid epidemic in America and the fact that the majority of deaths have been driven primarily by fentanyl contamination, the CDC and NIH have both stated that they do not expect a significant reduction in deaths by overdose this year. This situation is dire and will continue to be dire for some time to come.
Coping with opioid overdoses will require people to come together, push further, and implement new structures to help people with treatment of substance abuse disorders. The current model of criminalization and treatment has led directly to the situation that we find ourselves in today. It will not go away until our way of treating addiction evolves to cope with the realities of the situation.
One area that could be expanded is helping people find alternate ways to deal with the stresses of their lives that don’t involve substance use. It may seem oversimplified, but helping people train themselves to redirect impulses to dwell in stress towards physical activities like sports, jogging, walking or social interactions like games, calling friends, or the like can seriously help people avoid substance use. These have been less available during the pandemic, due to the risk of catching COVID-19, but will prove to be a crucial part of our recovery as a nation in the long term. We would do well to build plans on how to expand this literacy, and to build activities and systems of interaction that are resilient to future pandemic level threats as we rebuild.
Direct aid to the public at large could also do quite a lot to reduce stress that causes people to turn to substances in the first place. By strengthening the safety net, giving parents more direct aid, and reducing the threat of homelessness or hunger, governments and communities alike can remove many of the most basic stresses from people.
It is hard to directly counter the threat of fentanyl contamination but testing programs like those in California have shown positive results in reducing harm to people as they are working on recovering from a substance use disorder by allowing them to, at the very least, avoid harmful cases of contamination that might kill them.
Talk To A Professional if You Need Help With Addiction

We started our substance use disorder program in Albuquerque to help meet the growing demand for affordable addiction recovery services in our area. Our goal is to help as many people as we can. We know recovery is possible and overdose is preventable. If you or someone you know is having trouble, please reach out. We’re here to help.